Prostate Artery Embolisation
Prostate Artery Embolisation
Prostate Artery Embolisation (PAE) represents a sophisticated, minimally invasive intervention for Benign Prostatic Hyperplasia (BPH), adapting established Interventional Radiology techniques to address this common condition. Arterial embolisation methodologies have been successfully implemented for several decades across diverse clinical scenarios, including haemorrhage control, management of uterine fibroids, and treatment of renal and hepatic neoplasms.
The therapeutic mechanism of PAE centres on precisely interrupting the arterial blood supply to the prostate, predominantly targeting the centrally enlarging tissue that impinges upon the urinary pathway. As blood perfusion diminishes, the hypertrophied prostatic tissue undergoes relaxation and controlled atrophy, effectively alleviating pressure on the urethra. This physiological response manifests clinically as significant improvement or complete resolution of Lower Urinary Tract Symptoms (LUTS), restoring normal urinary function and enhancing quality of life.
Procedural Details
Prostate Artery Embolisation (PAE) is performed as a day procedure in an advanced Interventional Radiology suite, typically within a hospital setting. The procedure utilises local anaesthesia, sometimes complemented by mild sedation for patient comfort.
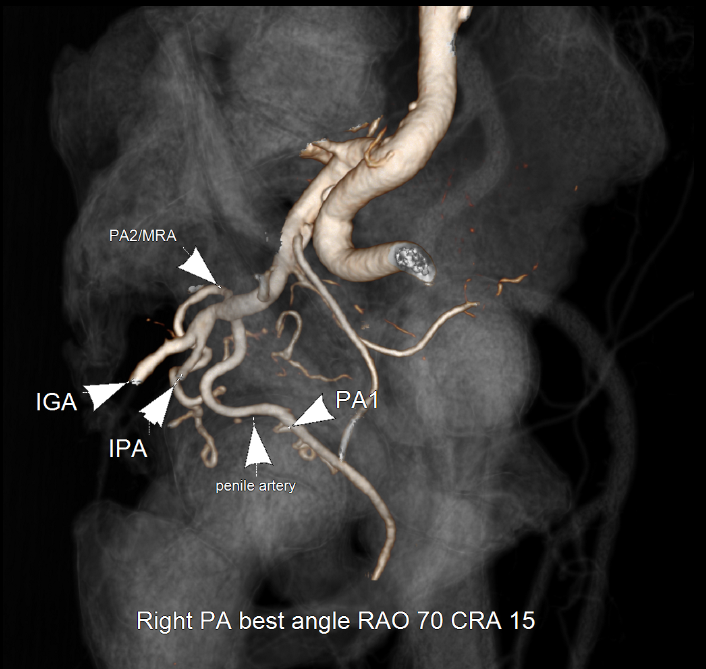
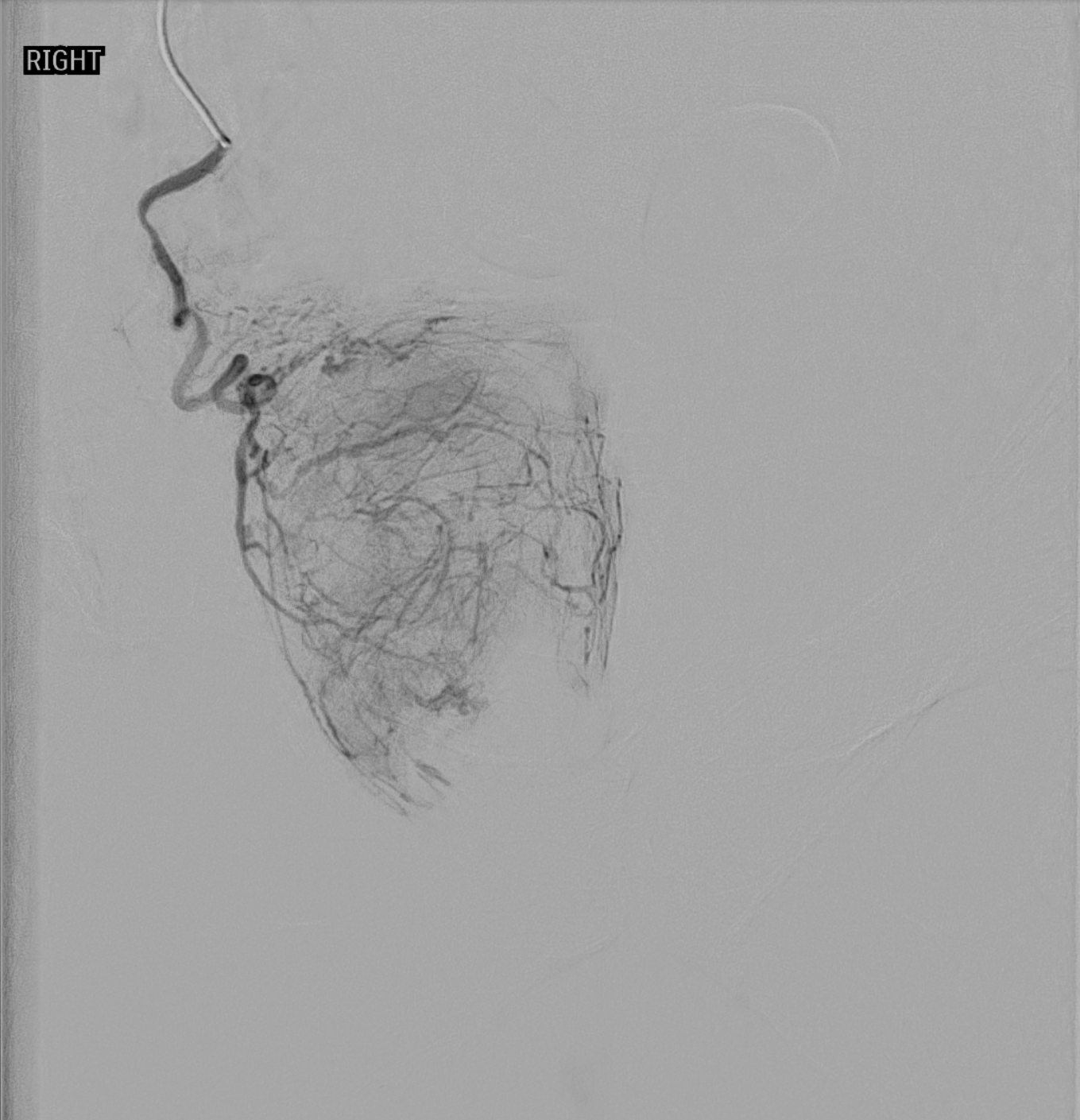
Access to the arterial system is gained via either the right femoral artery (groin) or left radial artery (wrist). A small catheter is precisely navigated toward the prostatic arteries using sophisticated digital imaging technology. Upon reaching the target prostatic artery, a specialised microcatheter is deployed to perform the embolisation. Fine embolic particles or medical-grade adhesive are then methodically introduced into the prostatic arterial branches, effectively occluding blood flow to the hypertrophied prostatic tissue. This process is subsequently repeated for the opposite prostatic artery to ensure comprehensive treatment.
The procedure typically requires 90-120 minutes to complete. Patients remain conscious throughout and may observe the intervention on high-resolution monitoring screens. Following completion, the vascular access sheath is removed, and controlled compression is applied to the entry site before placement of a compression dressing. Patients who undergo the radial approach may ambulate almost immediately, while those with femoral access typically mobilise after a four-hour recovery period. Patients are encouraged to void post-procedure while medical staff continuously monitor their recovery. Discharge typically occurs the same day, in accordance with the Interventional Radiologist's clinical assessment and recommendation.
How long do I have to remain in hospital?
Generally, patients are admitted 1-2 hours prior to the embolisation procedure and discharged the same day, typically 2-6 hours post-procedure.
What are the risks associated with PAE?
Most patients experience no symptoms during the procedure. Following treatment, some may experience mild pain, burning sensation, or urinary frequency, which are readily managed with appropriate medication and typically resolve within 7 days.
Common complications include those associated with any arterial catheterisation, predominantly haematoma or bruising at the puncture site. Less common complications include minor haematuria or urinary tract infection, which is effectively prevented through prophylactic antibiotic administration before and after the procedure. Very rare complications include temporary haematospermia, though these adverse symptoms typically resolve spontaneously within days.
Occasionally, patients with severe BPH may require temporary urinary catheterisation, which can usually be removed on the day of or shortly after attending a trial of void clinic.
Can I be treated regardless of the size of my prostate?
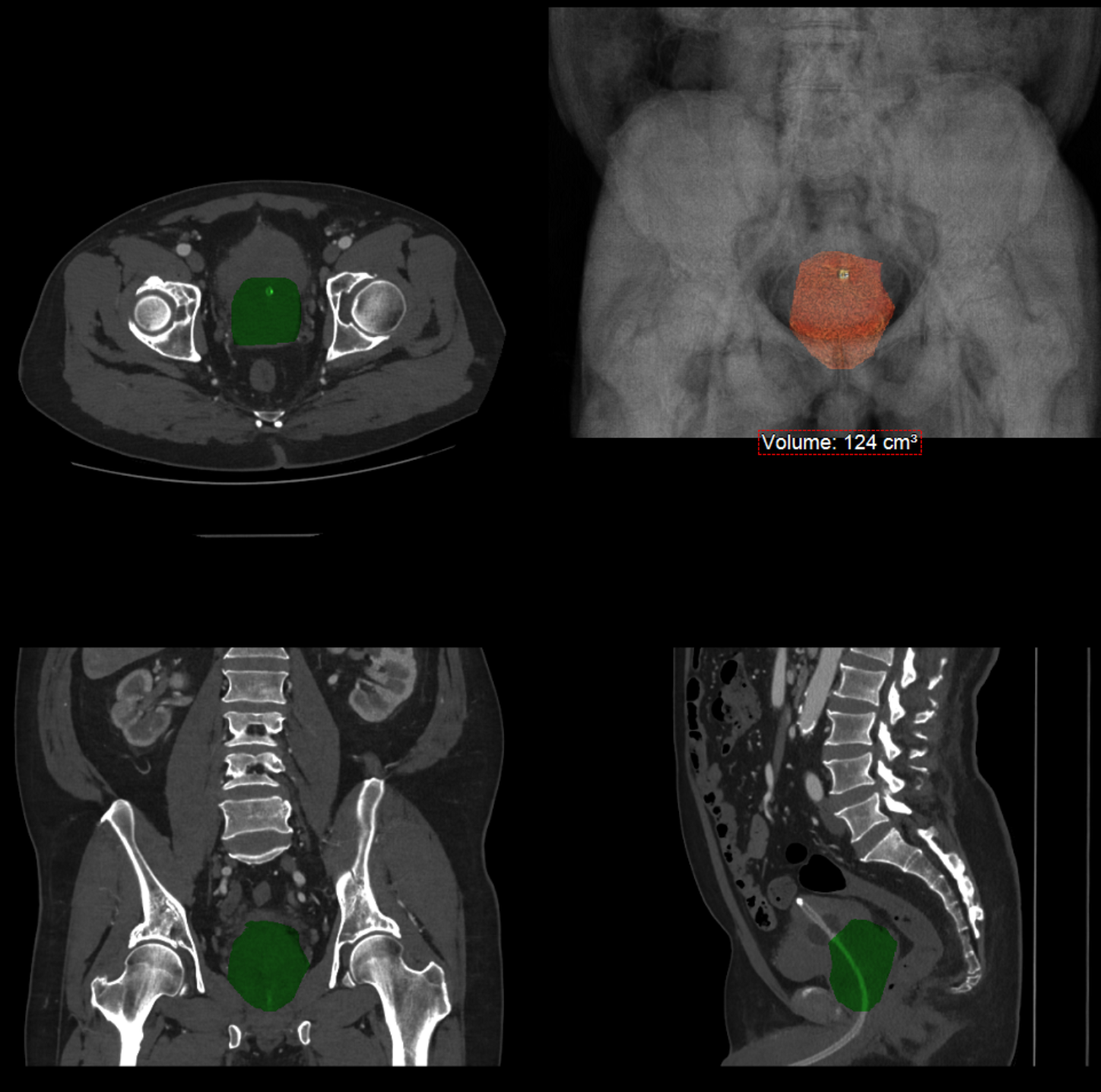
Prostatic Artery Embolisation is performed only when symptomatic Benign Prostatic Hyperplasia is present. The procedure is suitable even for significantly enlarged prostates exceeding 200cc in volume. However, if your prostate volume is less than 40cc, you may not meet the treatment criteria.
Will my sexual function be affected?
Current research indicates that patients undergoing PAE for BPH do not experience decline in sexual function. Sexual dysfunction is more commonly associated with side effects from prescription medications previously used to manage BPH symptoms prior to PAE intervention.
What happens to the prostate after embolisation?
Embolisation typically results in gradual prostate volume reduction ranging from 10-50%. Notably, approximately 20% of patients experience symptomatic improvement without measurable changes in prostate size, potentially due to reduced intraglandular pressure (currently under investigation).
The primary objective of embolisation is symptomatic improvement rather than volume reduction, though the latter occurs in most patients as a consequence of atrophy of the abnormal central gland tissue.
Can my BPH be treated by PAE?
PAE may be appropriate if the following criteria are met:
The BPH is causing clinically significant symptoms (IPSS score greater than 8)
The prostate volume exceeds 40cc
Peak urinary flow (Qmax) is less than 12mL/sec
No contraindications are present
What are the contraindications for PAE?
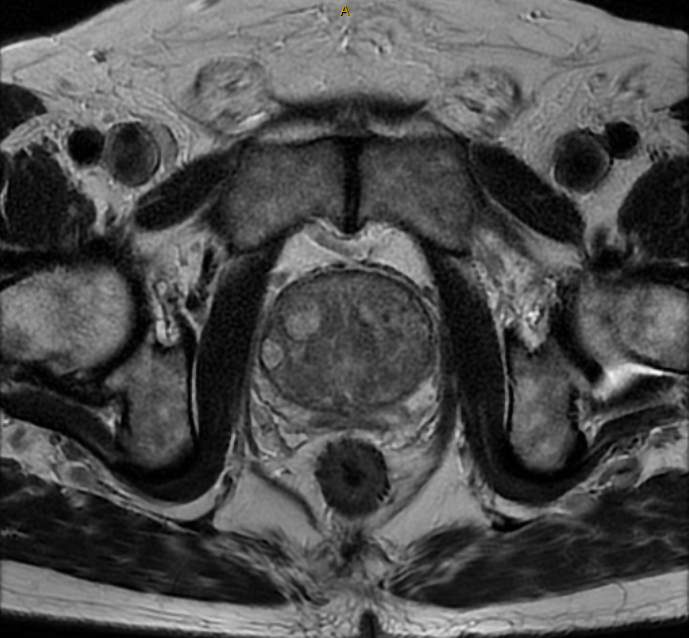
Prostate cancer is the main contraindication for PAE. This is screened for with a prostate MRI prior to all PAE procedures.
Minimally symptomatic patients may not benefit from PAE (IPSS less than 8).
Anaphylaxis to contrast media.
Unsuitable arterial anatomy which can be any combination of:
Excessively tortuous (twisted) pelvic or prostatic arteries.
Severe pelvic or prostatic artery stenoses (narrowings).
Prostate arteries too small to catheterise with a microcatheter.
What are the next steps for my PAE?
After scheduling a consultation with an Interventional Radiologist, several assessments will be arranged. Patients complete standardised questionnaires including the International Prostate Symptom Score (IPSS), Quality of Life assessment, and Sexual Health Inventory for Men (SHIM) survey.
During consultation, more specialised tests may be performed, including ultrasound and urodynamic flow studies. Based on these results, suitability for PAE will be determined.
If embolisation is considered appropriate, prostate MRI and high-quality CT angiography will be required to evaluate pelvic vasculature and confirm candidacy. Left arm vasculature will also be assessed.
Following these examinations, the Interventional Radiology team will contact you regarding the scheduled procedure date.