MRI Guided Cryoablation
The Future of Minimally Invasive Cancer Treatment
Our doctors at Spectrum Interventional Radiology are Australia's most experienced cryoablation experts, with over a decade of expertise and hundreds of successful procedures. At Liverpool Hospital, our team is the only group in Australia offering MRI-guided cancer intervention, with cryoablation for solid organ tumours, bone lesions, vascular malformations, and nerve treatments.
This page explains what cryoablation is, how MRI guidance works, and whether this treatment might be right for you.
What Is Cryoablation?
Cryoablation is a minimally invasive treatment that destroys tumours and other abnormal tissue by freezing. Instead of surgically removing a tumour, a thin needle (called a cryoprobe) is placed directly into the target through a small skin puncture, guided by imaging. The needle tip then reaches temperatures as low as minus 140 degrees Celsius, forming a ball of ice that destroys the targeted tissue.
Cryoablation has been used safely and effectively for over a decade at Liverpool Hospital to treat cancers, benign tumours, vascular malformations, and chronic pain conditions. We can also perform the procedure at Sydney Southwest Private Hospital, and other public hospitals where our team hold appointments including Concord Hospital and Prince of Wales Hospital.
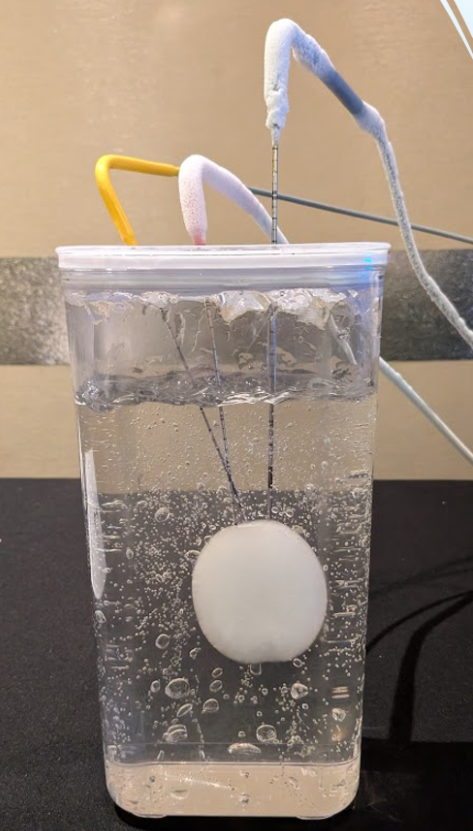
Cryoablation probes being tested in one of our workshops. Note the giant ice ball formed here, the size of a small mandarin.
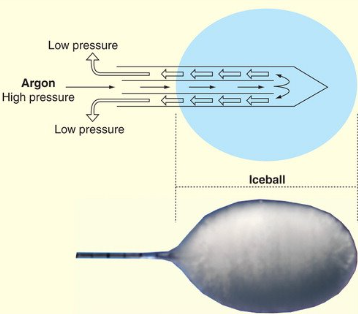
How Does Cryoablation Work?
The cryoprobe uses compressed argon gas. When this gas is released at the needle tip, it expands rapidly, causing an extreme drop in temperature — a principle in physics known as the Joule-Thomson effect. You may have noticed a mild form of this yourself, when using a can of deodorant. This creates a growing ball of ice around the needle tip.
The ice destroys cells through several mechanisms. During freezing, ice crystals form in and around cells, damaging cell membranes and internal structures. Water also rushes out of cells during freezing, dehydrating them. During thawing, water rushes back into damaged cells, causing them to swell and burst. For cancerous tumours, two complete freeze-thaw cycles are typically performed to ensure thorough treatment. Each cycle takes approximately 30 minutes.
Depending on the size and location of the target, typically two to four cryoprobes are positioned so that their ice balls overlap and fully cover the lesion.
Advantages of Cryoablation
Cryoablation offers several important benefits compared to surgery and heat-based ablation techniques such as radiofrequency and microwave ablation.
The ice ball is directly visible on imaging during the procedure. Your interventional radiologist can watch it grow in real time, confirming that the treatment zone covers the entire target. By contrast, heat-based ablation zones cannot be directly seen — the extent of treatment must be estimated based on isotherm charts.
Cryoablation preserves the structural framework of tissue. While the cells within the ice ball are destroyed, the underlying collagen scaffolding is maintained. This allows normal tissue to heal and regenerate along the preserved framework. Blood vessels within the treated area often recover their function. This is particularly important because it means cryoablation carries a much lower risk of causing strictures — narrowing of tubes such as bile ducts, the ureter, or airways — compared to heat-based ablation.
Extreme cold has a natural numbing effect. Many patients find the procedure no more uncomfortable than a needle biopsy. Unlike heat-based ablation, which typically requires general anaesthesia, cryoablation can often be performed with conscious sedation or even local anaesthesia alone. This makes it accessible to patients who may not be suitable for general anaesthesia.
Cryoablation is repeatable. Because it causes minimal scarring and preserves tissue architecture, it can be performed again if a tumour recurs or if new lesions develop. There is no upper limit to the amount of times cryoablation can be repeated unlike surgery and radiotherapy.
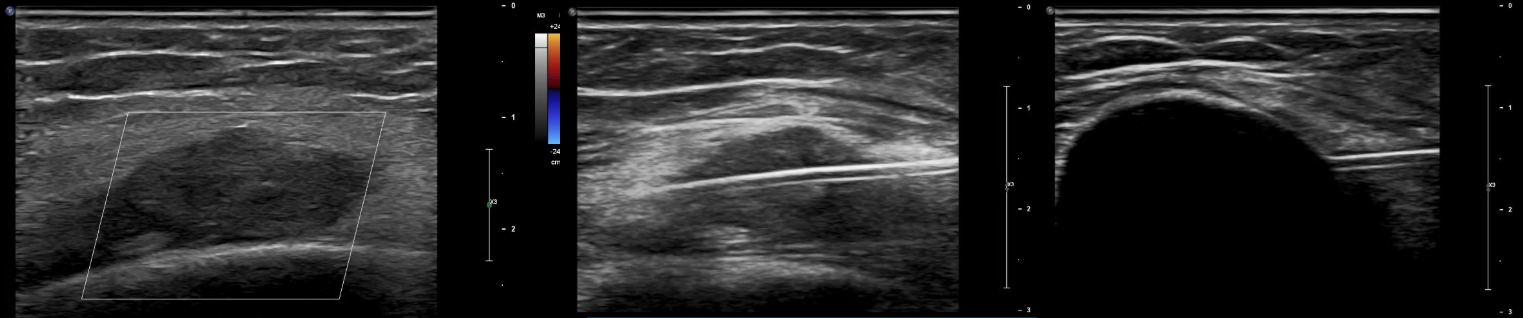
A symptomatic venous malformation is treated with cryoablation using ultrasound guidance. The left image shows the lesion under ultrasound. The middle image shows placement of a cryoprobe through the lesion. The right image shows formation of an ice ball completely covering the lesion.
What Is MRI Guidance?
For many years, cryoablation at Liverpool Hospital has been performed using ultrasound and CT guidance — well-established imaging methods that work well for most cases. Recently, we have added MRI guidance to our capabilities.
It is important to understand that the MRI machine does not perform the freezing. It is purely an imaging tool that allows your interventional radiologist to see exactly where the needle is and how the ice ball is forming, with exceptional detail.
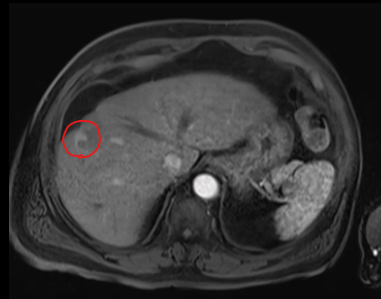
MRI provides the best soft tissue contrast of any imaging modality. Some tumours are invisible on ultrasound and CT but clearly visible on MRI. For these lesions, MRI guidance is the only way to accurately place the cryoprobe into the target.
MRI also allows needle placement along any angle, provides imaging in any plane, and uses no radiation — making it particularly suitable for younger patients and difficult locations. The ice ball appears as a clearly defined hypointense (dark) region on all MRI sequences, and its relationship to nearby structures can be monitored with millimetre precision.
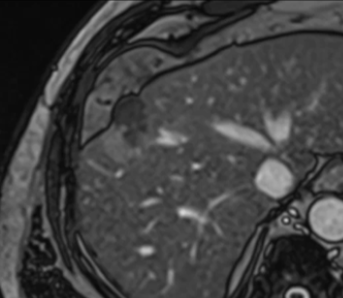
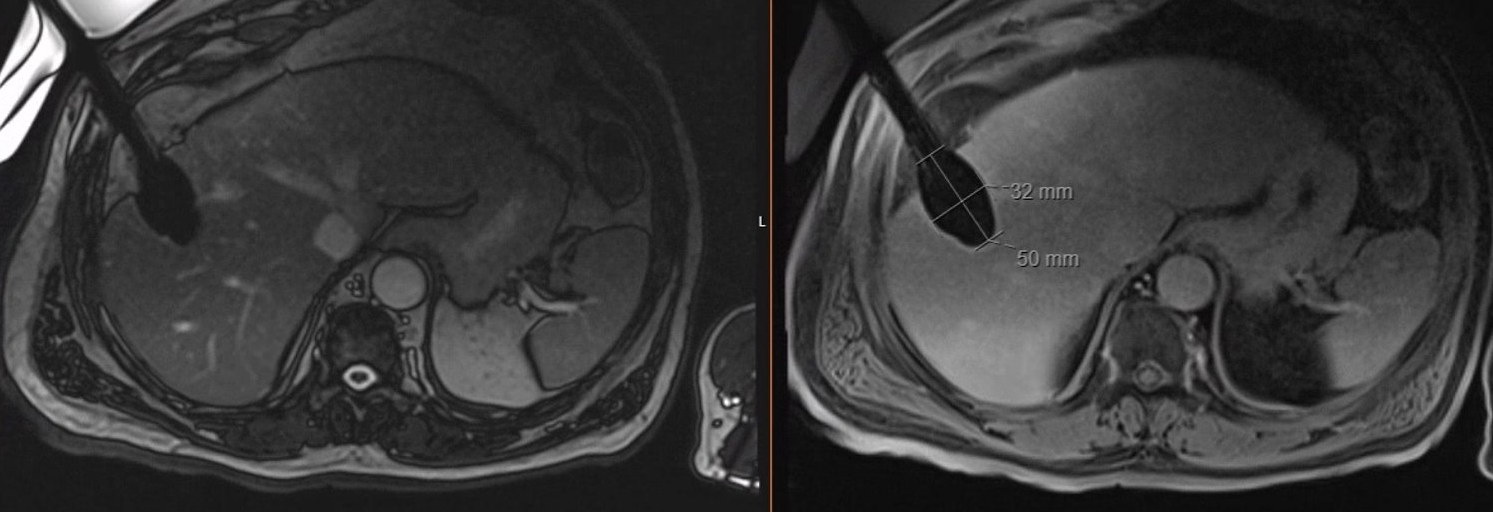
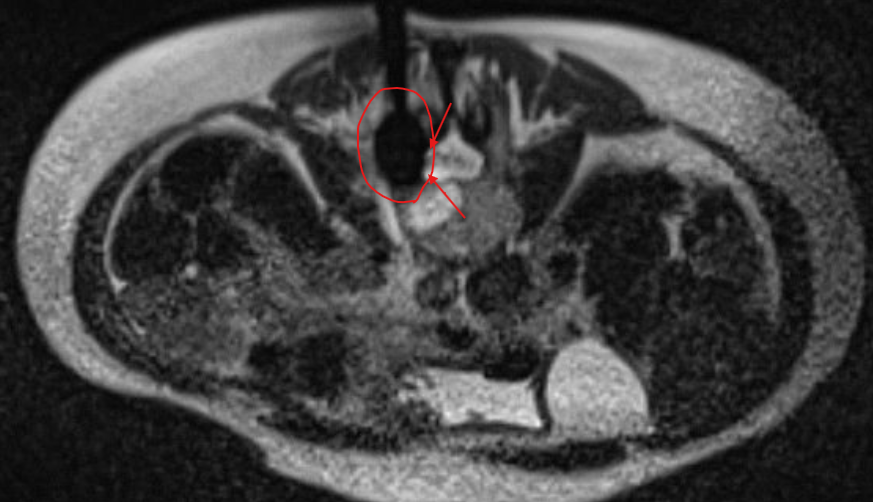
A small hepatocellular carcinoma is shown on MRI. It demonstrates arterial enhancement after gadolinium injection.
The same lesion is visible on non-contrast MRI (Trufi), ensuring easy targeting with MRI guidance.
Real-time MRI guidance is used to place the first cryoprobe into the lesion.
The ice ball is well visualised on all MRI sequences, ensuring complete coverage of the tumour with margins to spare.
When Is MRI Guidance Used?
MRI guidance is not always necessary. If a lesion is well seen on CT or ultrasound, those modalities are effective and often faster. MRI guidance adds the most value in specific situations.
Lesions that are invisible on other imaging are the primary indication. Some kidney tumours are endophytic (grow inward) without changing the kidney's outer shape, making them difficult to see on CT or ultrasound. Certain liver lesions are only visible on non-contrast MRI, requiring contrast on US or CT to image. In these cases, MRI guidance is the best way to accurately target the tumour.
Lesions near critical structures benefit from MRI's superior soft tissue detail. An example would be a bone tumour immediately adjacent to the spinal cord. This can only be safely treated using MRI guidance — which lets us watch the ice ball approach but not contact the spinal cord in real time.
Benign conditions such as venous malformations and endometriomas are extremely well characterised on MRI, making it an ideal guidance modality for their treatment.
Current limitations of MRI-guided cryoablation include a maximum treatable lesion size of approximately 3.5 cm (as MRI-compatible probes create smaller ice balls than standard probes) and the requirement that patients have no contraindications to MRI, such as certain older pacemakers or metallic implants.
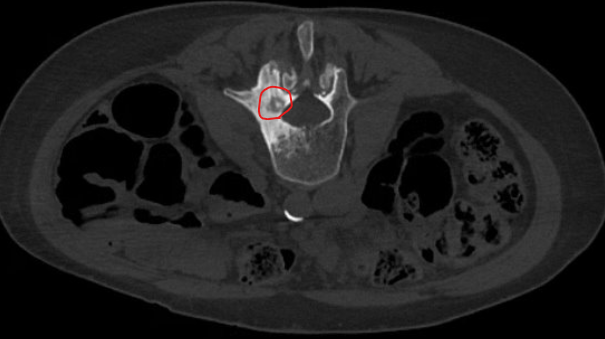
A painful bone lesion known as an osteoid osteoma is seen here in a lumbar vertebra. Note the close location to the spinal canal.
MRI guided cryoablation allows easy visualisation of the ice ball (red circle) allowing our team to stop the freeze once the ice neared the nerve roots in the spinal canal (red arrows). This level of precision is not available with any other imaging modality.
What Can Cryoablation Treat?
Cryoablation is used to treat a range of conditions across oncology, pain management, and benign disease.
Kidney cancer is one of the most established applications. For small renal cell carcinomas, cryoablation achieves success rates from 90-98% It is recognised as an appropriate treatment option for tumours <3 cm in the American Urological Association guidelines, particularly for patients who are high risk for surgery, have a solitary kidney, or prefer a minimally invasive approach.
Liver tumours, including hepatocellular carcinoma and metastatic disease, can be effectively treated. Multiple studies demonstrate similar efficacy between microwave ablation, radiofrequency ablation, and cryoablation with cryoablation having the most favourable complication profile. Our team also combines cryoablation with tumoural embolisation with Lipiodol tagging or TACE to create a synergistic effect leading to the best possible outcomes for liver cancer.
Lung tumours, both primary and metastatic, can be treated in patients who are not candidates for surgery. Our team has performed a leading number of lung cryoablations in Australia.
Bone lesions including painful osteoid osteomas and bone metastases respond well to cryoablation. For metastatic bone disease, cryoablation is often combined with cementoplasty — injection of bone cement to provide structural reinforcement and additional pain relief.
Soft tissue tumours such as extra-abdominal desmoid tumours (aggressive fibromatosis) can be treated with cryoablation. Notably, cryoablation does not appear to trigger the aggressive regrowth that can sometimes follow surgical removal of desmoid tumours.
Vascular malformations, particularly venous malformations, are well suited to cryoablation, especially with MRI guidance.
Abdominal wall endometriomas, which can develop in surgical scars after caesarean section, can be treated with cryoablation as a minimally invasive alternative to surgical excision.
Cryoneurolysis — the targeted freezing of nerves — is used to treat chronic pain conditions. Because cryoablation preserves the nerve sheath while disrupting the nerve fibres, nerves can potentially regenerate, and the risk of painful neuroma formation is the lowest of any nerve ablation technique. Applications include treatment of cancer pain (splanchnic and intercostal nerve ablation), knee pain from osteoarthritis (genicular nerve ablation), Morton's neuroma, trigeminal neuralgia, amputation stump neuromas, shoulder pain, and hip fracture pain in patients who cannot undergo surgery.
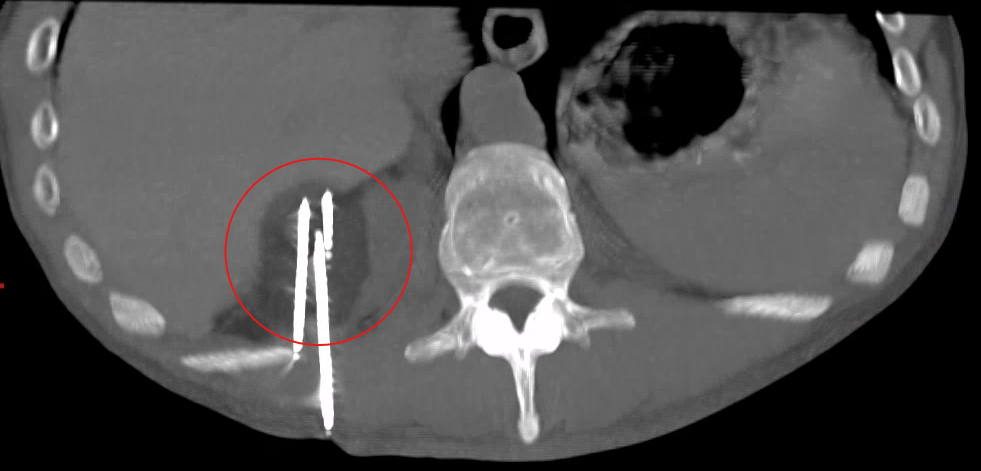
A small renal tumour is noted in the right kidney here. The patient was medically unfit for nephrectomy but still wanted curative treatment.
Three cryoprobes are placed into the lesion using CT guidance and the ice ball is seen to completely cover the lesion. The procedure was performed with local anaesthesia only and patient discharged home same day.
What Cryoablation Cannot Treat
Cryoablation is not suitable for all cancers or all situations. Cryoablation is not appropriate for cancers of hollow organs such as the bowel, stomach, bladder, or oesophagus, because freezing the walls of these organs would cause perforation.
Tumours immediately adjacent to the brain or spinal cord generally cannot be treated, although lesions near — but not directly involving — the spinal cord may be treatable with careful MRI-guided monitoring.
Diffuse or infiltrative tumours without clear margins are not suitable, as it is not possible to ensure adequate coverage.
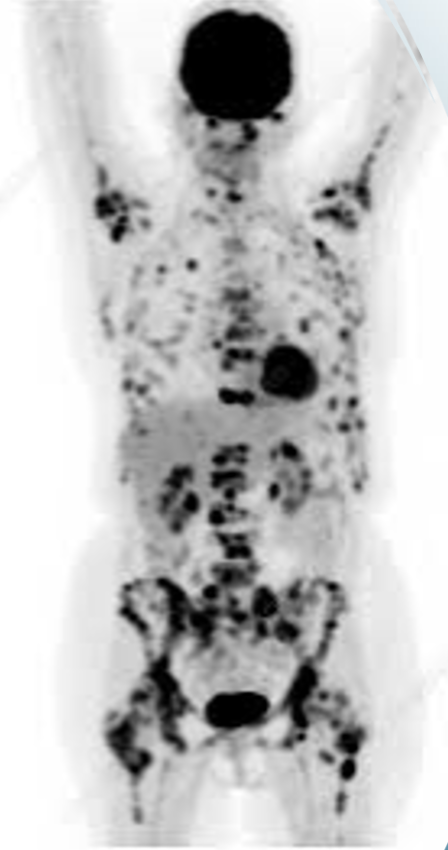
Cryoablation is best for treating one to two lesions per session. Patients with widespread metastatic disease involving many lesions are generally better served by systemic treatments such as chemotherapy or immunotherapy. However, even in advanced disease, cryoablation can play a valuable palliative role — particularly for pain relief from bone metastases or nerve-related cancer pain.
PET scan showing extensive metastatic disease, not amenable to treatment with cryoablation.
What to Expect
Most cryoablation procedures are performed with conscious sedation, meaning you are relaxed and comfortable but not under general anaesthesia. The main discomfort is from the initial needle placement, which is similar to having a biopsy. General anaesthesia is available if needed or preferred.
Procedure time is typically 90 minutes to two hours, depending on the number of needles required and the complexity of the case.
Most patients are discharged the same day or after an overnight stay. Return to normal activities is typically within two to seven days, with some restriction on heavy lifting for one to two weeks.
Follow-up imaging is performed at intervals — usually at three, six, and twelve months — to confirm successful treatment. On imaging, a successfully treated lesion shows no enhancement with contrast on CT or MRI, indicating no remaining viable tumour.
Overall complication rates are generally lower than surgery. The most common issues are minor pain at needle insertion sites and bruising. Significant complications such as bleeding requiring treatment or injury to adjacent structures are uncommon.
The team in action at Liverpool Hospital during an MRI guided case.
Our Experience
Our team has over ten years of experience performing cryoablation, with hundreds of kidney and liver cases completed. Our team has performed leading numbers of lung cryoablations and cryoneurolysis procedures in Australia. Dr Glen Schlaphoff and Dr Hao Xiang are the two lead interventional radiologists in the cryoablation space within our team. In addition the entire Spectrum IR team is experienced in cryoablation liver, renal and soft tissue masses.
Dr Schlaphoff and Dr Xiang regularly host cryoablation workshops for interventional radiologists from across Australia in partnership with Boston Scientific, and provide proctoring and consultation to centres establishing their own cryoablation programmes.
All oncological cases are discussed at multidisciplinary tumour board meetings involving surgeons, oncologists, radiologists, and other specialists. Cryoneurolysis cases for cancer pain are reviewed at a dedicated cancer pain multidisciplinary meeting.
Dr Glen Schlaphoff is the head of department of interventional radiology at Liverpool Hospital, a founding partner of Spectrum and the pioneer of cryoablation in Australia.
How to Access Treatment
Cryoablation requires a specialist referral. This is typically from an oncologist, surgeon, or relevant specialist depending on your condition. Your referral is reviewed by our interventional radiology team, your imaging is assessed for suitability, and if appropriate, a consultation is arranged to discuss the procedure, risks, benefits, and alternatives. Please ensure your referral includes your medical history, all relevant imaging (digital copies preferred), pathology results if available, and a list of current medications.
Depending on the clinical scenario, cryoablation can be performed at Sydney Southwest Private Hospital, or at public hospitals where our team has appointments including Liverpool Hospital, Concord Hospital and Prince of Wales Hospital. Please note that MRI guided cryoablation specifically is only available at Liverpool Hospital.